Our Stories Gallery | Takeda Pharmaceuticals

How we help innovative treatments reach more people
More than two centuries. Countless innovations. One vision.
From a single stall in an Osaka market to a global biopharmaceutical leader, we’ve always maintained a single set of values to guide our commitment to patients, our people and the planet.
And that has given us incredible stories to tell.

Considering quality of life when classifying psoriasis severity
January 16, 2026
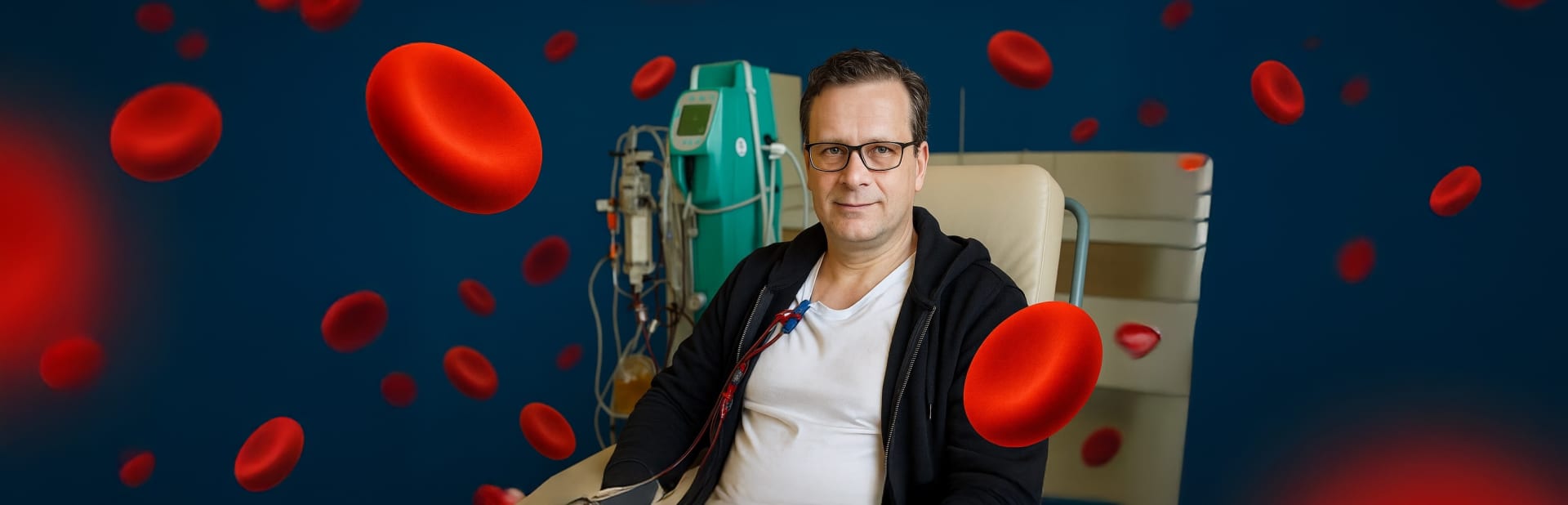
Facing the Unknown: Lucas’ Journey with iTTP
January 15, 2026

Unlocking education and opportunity for nurses
January 15, 2026

Bridging to the Future: Our Leaders Shaping a Bold New Chapter
December 22, 2025

How digitalization enables sustainable manufacturing
December 11, 2025

Setting sail – Pioneering sustainable transport of medicines by sea
November 14, 2025

Mentorship as multiplier: How mentorship strengthens communities
November 9, 2025

Climate-resilient health care: Our 2025 global CSR programs
September 24, 2025

The challenge of investigating the orexin pathway in narcolepsy type 1
September 19, 2025

Ito’s recipe for resilience with IBD
May 16, 2025

How we ‘level the playing field’ for small suppliers
April 28, 2025

From lost art to a lasting connection
April 17, 2025

Easing dietary challenges for IBD patients in Japan
April 17, 2025

Cultivating circular agriculture with a zoo in Japan
March 26, 2025

IBD patients embrace the everyday in European campaign
February 20, 2025

A first-of-its-kind collaboration to tackle health care emissions
February 10, 2025

Addressing the impact of climate change on child health
February 6, 2025

Understanding the root cause of inflammatory diseases
January 27, 2025
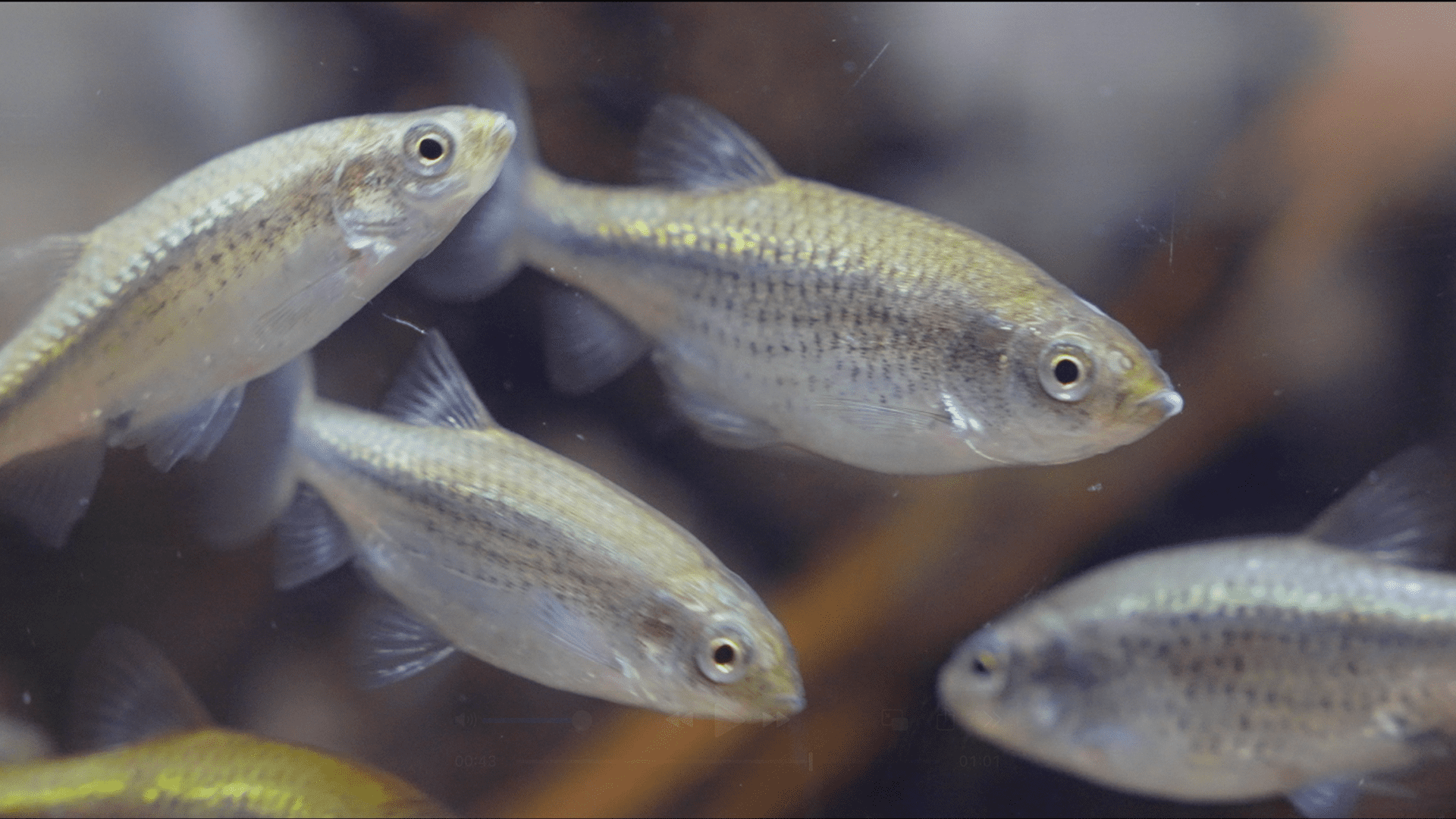
Small fish, big mission to protect biodiversity in Japan
January 23, 2025
Our approach to business development: Trust, agility, creativity
January 11, 2025

The impact of dengue: Two doctors’ perspectives
January 9, 2025
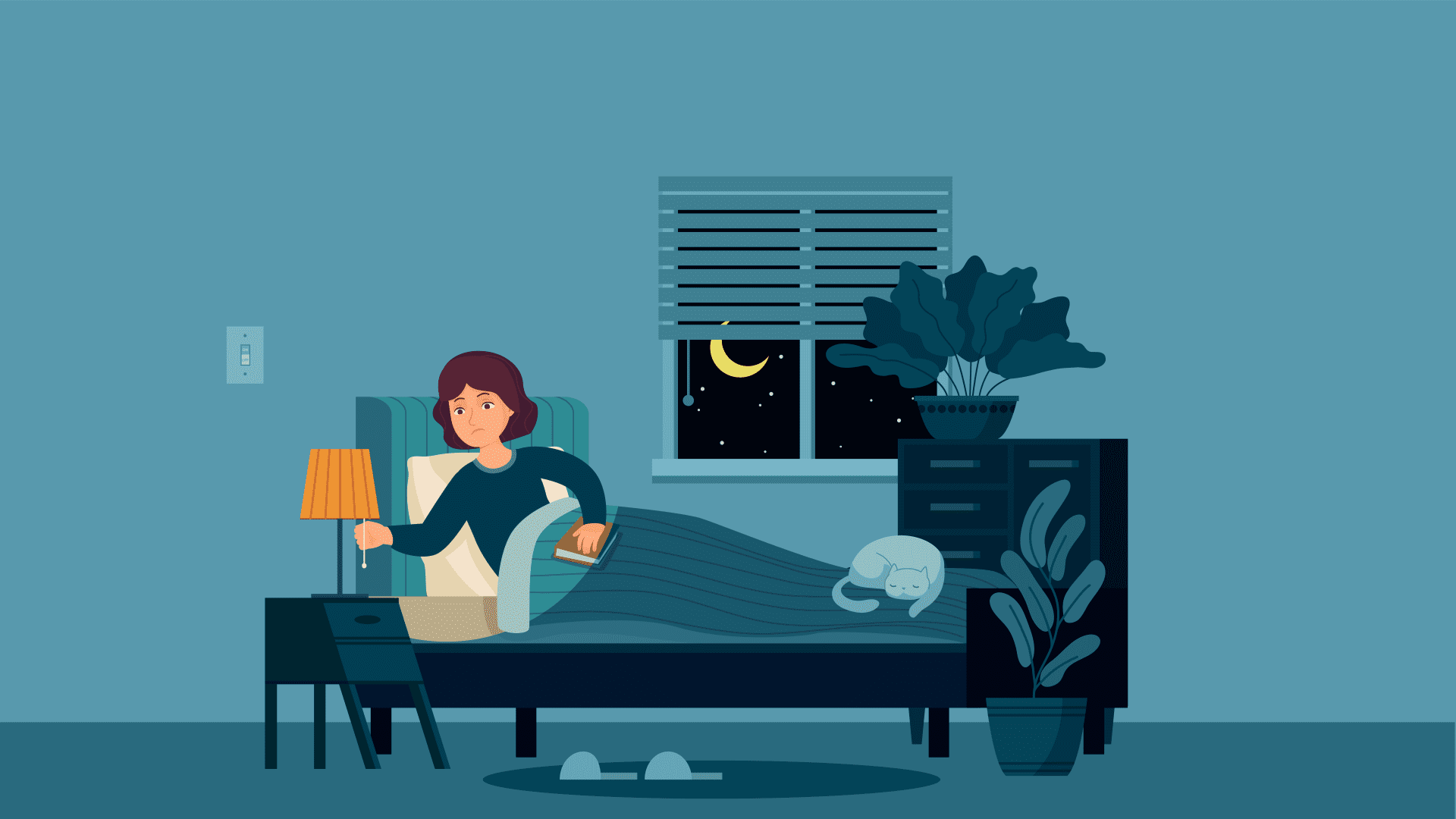
Driving innovation for narcolepsy type 1
December 19, 2024

Aiming to enhance regulatory submissions with GenAI
December 12, 2024

Joining forces to develop a multidisciplinary care model in GI
December 5, 2024

Innovative care navigators boost maternal health in India
December 5, 2024

Innovating to address neglected tropical diseases (NTDs)
November 14, 2024

Living with Psoriatic Disease: Stories of Resilience
October 25, 2024

Can wearable technology help in sleep disorder diagnosis?
October 17, 2024

Vaccine Business Unit leader's path began in dengue ward
October 17, 2024

In psoriatic arthritis, connections matter
October 9, 2024

From the heart: Meet our 2024 global CSR partners
September 19, 2024

Zambia’s first family medicine program overcomes the odds
September 19, 2024

Women, girls and health in the face of climate challenges
September 19, 2024

A new mother faces the challenge of the rare disease cTTP
September 12, 2024

Can Smart Technology help transform clinical trials?
September 12, 2024

The true burden of celiac disease: Bill’s journey
September 10, 2024

Preserving the 1,500-year-old hollyhock festival in Japan
September 4, 2024

Community Health Workers: Applying global lessons learned
August 29, 2024

How a conversation led to a new AI assistant
July 18, 2024

Community engagement to diversify clinical trials
June 25, 2024
![Picture of (Left to right): Junjing (Jane) Lin [Takeda], Hamaad Adam [MIT], Jianchang Lin [Takeda]](https://assets-dam.takeda.com/image/upload/c_lfill,w_1920/q_auto:eco/f_auto/v1/Global/Our-Stories/MIT-Takeda%20Program%20uses%20AI%20to%20unlock%20innovation/0019_MIT_Takeda_celebration_2024_019)
MIT-Takeda Program uses AI to unlock innovation
June 20, 2024

The burden of dengue and hope amidst hardship
June 13, 2024

Living with narcolepsy: Kelsey's story
June 12, 2024

Innovation in access reaches new heights
May 2, 2024

Haunted by dengue, she fights social inequities
April 29, 2024

Engaging patients at the Healthcare Café in Japan
April 18, 2024

Health inequity in rare disease: The long journey to diagnosis
February 29, 2024

Run Takeda Run
February 7, 2024

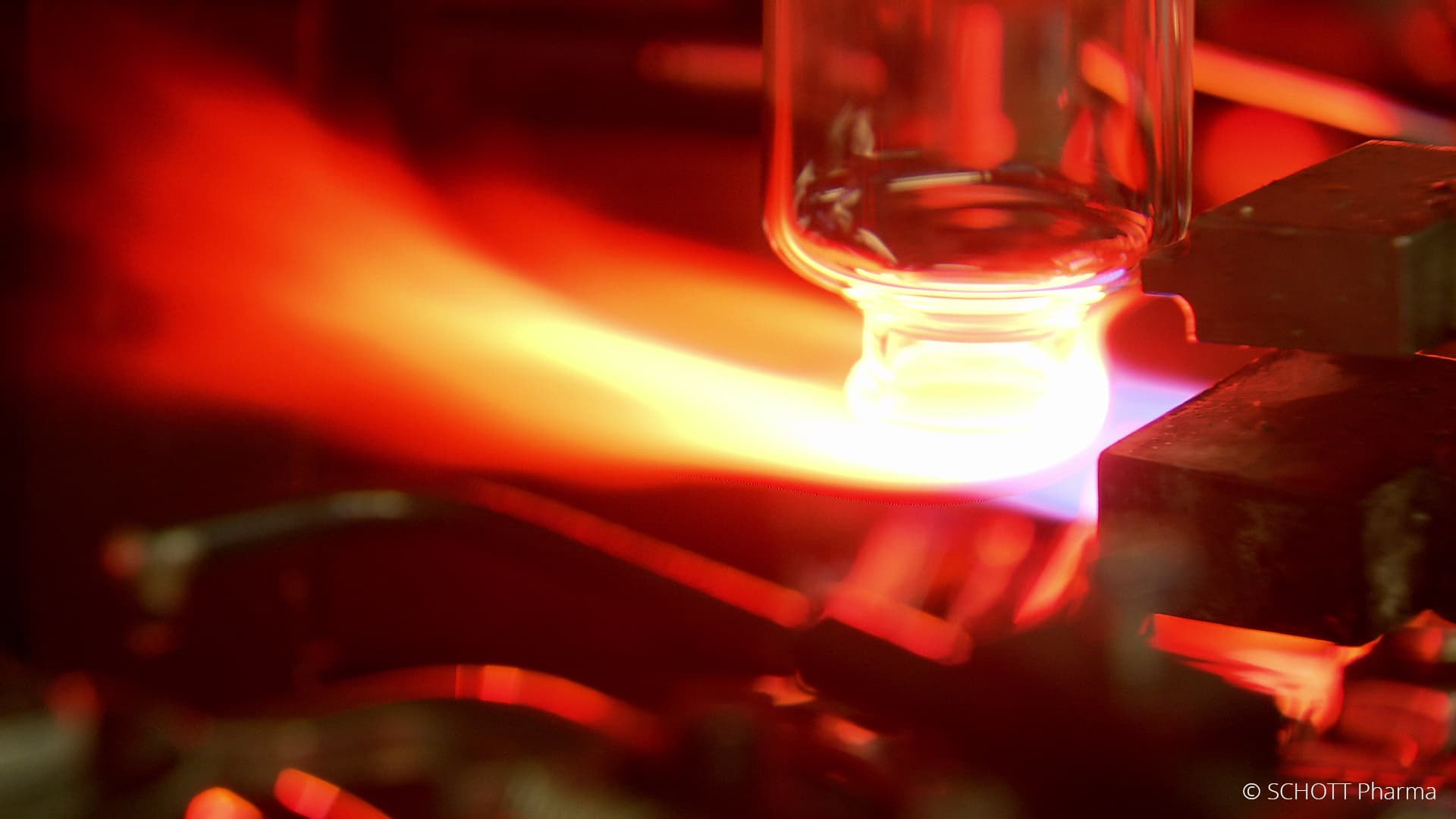
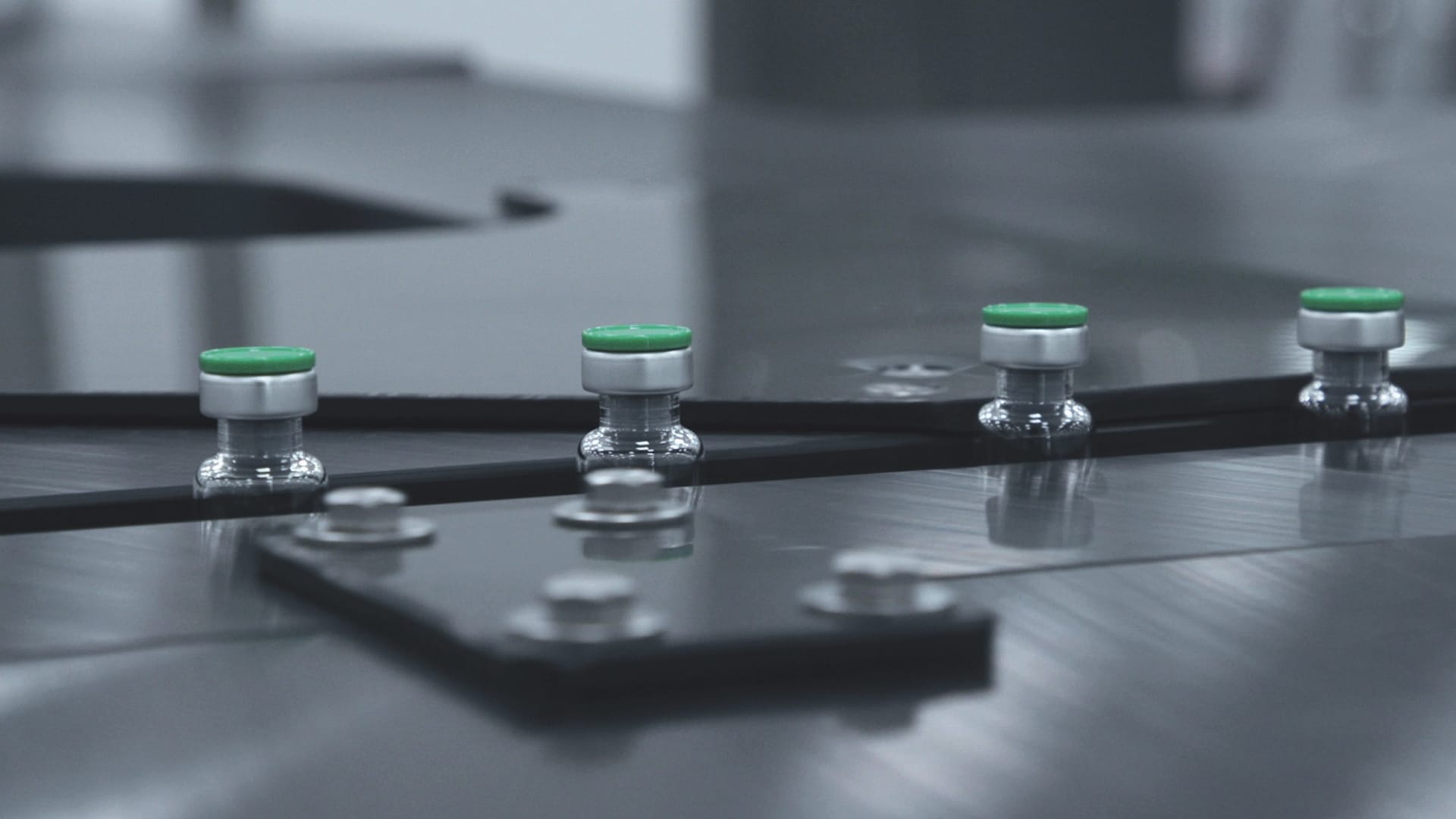
Pride in producing plasma-derived therapies
January 11, 2024

Offering IBD patients special recipes from Hyatt chefs
December 19, 2023

An unusual mural honors rare disease patients
December 14, 2023

Long-term partnership yields positive results for refugees
November 30, 2023

What drives our dengue researchers? Seeing the disease up close
November 2, 2023

Doing more in psoriasis starts with listening and learning
October 11, 2023

Hear from our 2023 Global CSR partners
October 4, 2023

Spotlighting research and innovation for patients with TTP
September 12, 2023

This new building produces more energy than it uses
September 7, 2023
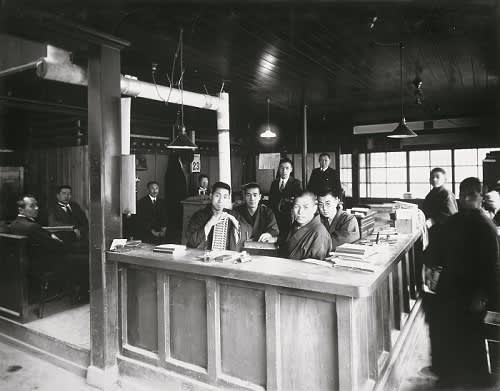
Integrity in the aftermath of a historic earthquake in Japan
August 31, 2023

R&D colleagues share their stories
August 7, 2023

A father's experience with dengue
June 15, 2023

Takeda’s focus on health equity: Rare Disease Day 2023
February 25, 2023

Pursuing life-transforming science
January 17, 2023
A digital transformation to make a global impact
November 9, 2022

Harnessing science to push the boundaries of what’s possible
September 21, 2022

Integrating data sciences into clinical development
September 19, 2022

Training health workers to reach remote communities
March 9, 2022

Evi found a team who makes her feel heard
February 10, 2022

Innovation is key to sustaining our business
December 15, 2021

Improving the health of ethnic minority women and newborns in Asia
November 17, 2021

Elvis brought a global vision to his home office
June 12, 2021

For Aki, "Takeda-ism" is a family affair
June 9, 2021

Universal Health Coverage and the power of people: UNGA side event
November 21, 2019

Transforming global child health research with the LSHTM
August 8, 2019

Shared knowledge for a better life for all
November 9, 2018

Shonan Health Innovation Park ("Shonan iPark")
April 18, 2018

Health care for all
January 15, 2017