Health inequity in rare disease time to diagnosis | Takeda Stories

Health inequity in rare disease: The long journey to diagnosis
This article includes real-life patient experiences. Individual experiences may vary. This information is available to the general public for informational purposes only; it should not be used for diagnosing or treating a health condition or disease. It is not intended to substitute for consultation with a health care provider. Please consult your health care provider for further advice.
Janice Strydom was a 15-year-old living in South Africa when she began the arduous journey of diagnosis – which is unfortunately shared by many people living with a rare disease. She first noticed a swelling in her hand. The next day, the severity of the swelling had increased, which doctors attributed to a spider bite. In the following years, she experienced swellings every other week, including her face, stomach, and feet.
She was 21 before doctors uncovered the actual cause – hereditary angioedema (HAE), an under-recognized, rare, genetic condition resulting in the accumulation of excessive fluid in different parts of the body.
“From the first attack until the time that I got a definitive diagnosis, it was six years,” says Janice. “It feels a lot longer when you’re going through that pain, and not knowing what’s wrong.”
Her experience is not unique. Janice is one of 300 million people impacted by rare diseases.1,2 One of the greatest health inequities the rare disease community faces is the length of the diagnostic journey, which can vary in different disease areas. The average time to receive an accurate diagnosis of a rare disease is 4-5 years, but in some cases like in 50% of those with HAE, it can take over a decade.3,4,5,6,7
Where you live can be crucial to receiving a diagnosis. Specialist treatment centers may not be geographically accessible, requiring people to travel long distances. The care gap between rural and urban communities can be vast,8 to which Janice can speak firsthand.
“There can be long distances to get to hospitals and there can be a lack of knowledge of the disease,” she says. Diagnosis can also involve multiple interactions with different specialists. “You need a doctor who has the time and knowledge and is prepared to look into what’s wrong.”
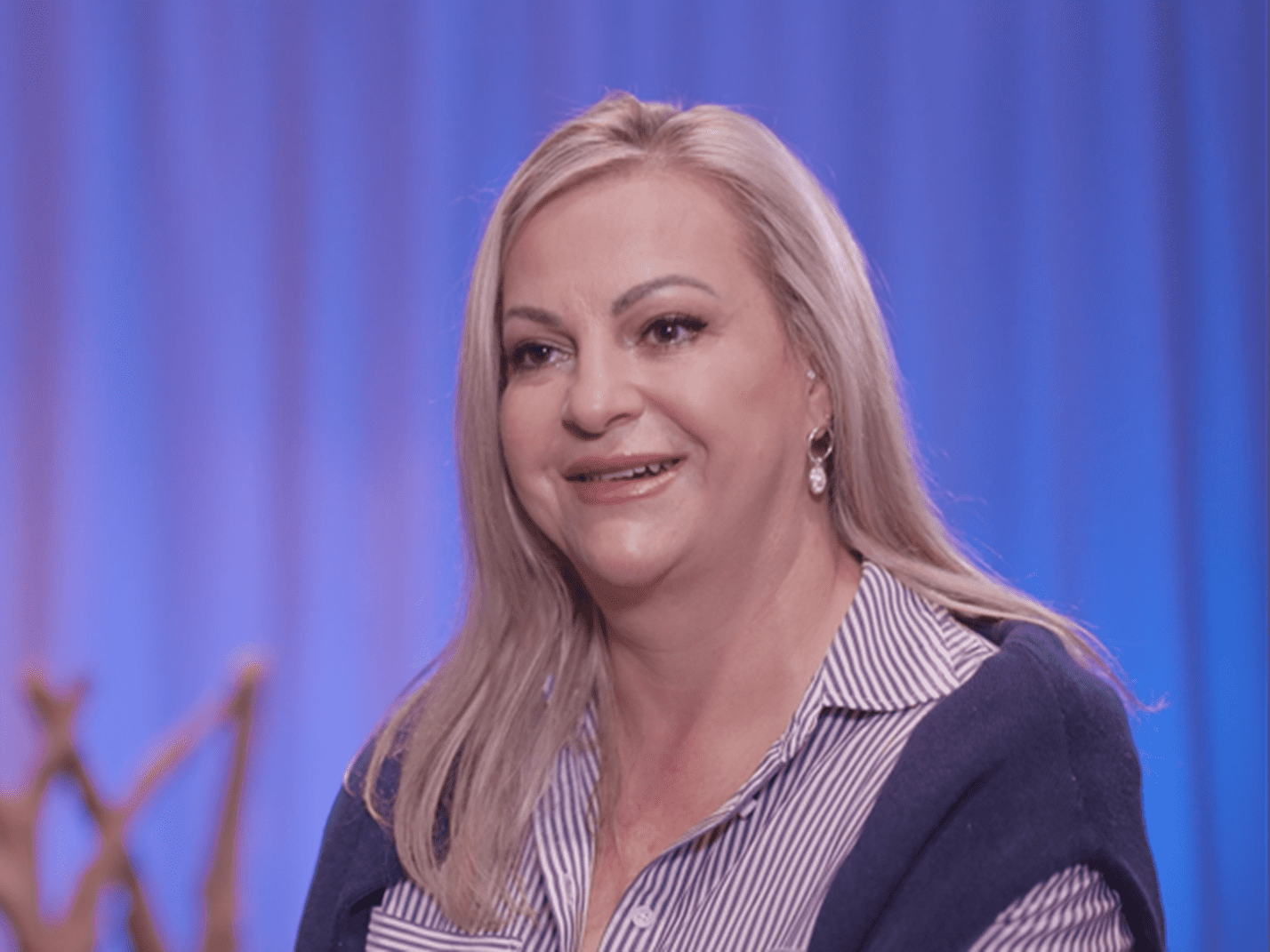
“From the first attack until the time that I got a definitive diagnosis, it was six years. It feels a lot longer when you’re going through that pain, and not knowing what’s wrong.”
Janice Strydom, chief executive officer of HAE International South Africa
Takeda’s Head of Rare Diseases for Global Medical Affairs, Neil Inhaber, M.D., FRCPS, says the development of innovative diagnostic solutions has helped bring meaningful change for people with rare diseases, including HAE.
“Our in-house researchers have pioneered a simple but comprehensive dried blood spot test to support the timely diagnosis of HAE in places where multiple hurdles to prompt diagnosis, and sometimes even care, exist,” he says. “The SpotHAE program is being trialed in four countries – South Korea, China, Poland and Italy.”
Since its launch in 2022, more than 1,300 spot tests have been conducted in China alone, of which 30% were indicative of HAE.9 The program is helping to accelerate diagnoses and care for people who previously faced an uncertain diagnostic pathway.
“Our aim is to cut the diagnostic journey in half for people with HAE within the next 10 years,” says Neil. “However, we recognize the challenge of reducing health inequities for people with rare diseases cannot be achieved alone and requires a multifaceted approach.”
Björn Mellgård M.D., Ph.D., Takeda’s Global Program Lead, Rare Genetics and Hematology adds, “For the past two centuries, Takeda has been focused on innovation to address unmet patient needs. That innovation includes partnering with others who share our values.”
Björn points to one of our key partnerships with EURODIS, the non-profit alliance of more than 1,000 rare disease patient organizations from 74 countries. “EURODIS recognizes the importance of early intervention. Our partnership to launch the newborn screening project, Screen4Care, is one example of collaborations that are having impact,” says Björn.
Given the estimate that 80% of rare diseases have genetic origin, of which the majority affect children,10 Screen4Care aims to shorten the diagnosis journey via genetic screening and digital technologies.
Janice recognizes the importance of those early childhood connections. She now shares her knowledge to help others living with HAE, as the chief executive officer of the patient advocacy organization, HAE International (HAEi) South Africa.
“One of the focuses we have as a patient advocacy group is our children," she says. “So, we’re looking for solutions for those patients, to see what we do with those missing years.”
- Nguengang Wakap S, et al. Estimating cumulative point prevalence of rare diseases: analysis of the Orphanet database. Eur J Hum Genet 28, 165-173 (2020).
- Orphanet. New scientific paper confirms 300 million people living with a rare disease worldwide. [Internet; cited 2023 Dec]. Available from: https://download2.eurordis.org/pressreleases/PrevalencePaper_JointStatement_170919_Final.pdf
- Banerji A, et al. Current state of hereditary angioedema management: a patient survey. Allergy Asthma Proc. 36(3):213-7 (2015).
- Jolles S, et al. A UK national audit of hereditary and acquired angioedema. Clin Exp Immunol. 175(1):59-67 (2014).
- Marwaha S, et al. A guide for the diagnosis of rare and undiagnosed disease: beyond the exome. Genome Med 14, 23 (2022). Available from: https://genomemedicine.biomedcentral.com/articles/10.1186/s13073-022-01026-w#:~:text=The%20average%20time%20for%20accurate,decade%20%5B8%2C%209%5D
- Schöffl C, et al. Hereditary angioedema in Austria: prevalence and regional peculiarities. J Dtsch Dermatol Ges 17:416–423 (2019).
- Zanichelli A, et al. Misdiagnosis trends in patients with hereditary angioedema from the real-world clinical setting. Ann Allergy Asthma Immunol. 117:394–398 (2016).
- Adachi T, et al. Enhancing Equitable Access to Rare Disease Diagnosis and Treatment Around the World: A Review of Evidence, Policies, and Challenges. Int. J. Environ. Res Public Health 2023(2) 4732.
- Takeda data on file. Hereditary Angioedema spotHAE Report, Dec 2022-Oct 2023.
- Bick D, et al. Newborn Screening by Genomic Sequencing: Opportunities and Challenges. Int. J. Neonatal Screen 8, 40 (2022).
Related Stories
Takeda’s focus on health equity: Rare Disease Day 2023

